Abstract
Introduction: Cancer survivors are at risk for adverse mental and physical health outcomes. However, it is not well understood how these outcomes may be differentially experienced according to an individual's race and/or ethnicity. Historically marginalized racial and ethnic groups are at risk of experienced racism, and the subsequent negative mental and physical health consequences. We seek to evaluate associations of race, ethnicity, and experiences of racism, with adverse mental and physical health outcomes in survivors of cancer.
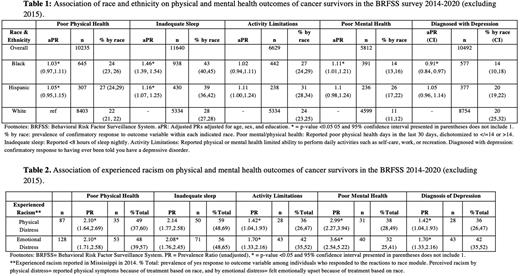
Methods: In this cross-sectional analysis using the Behavioral Risk Factor Surveillance System database, we evaluated data from 48,200 cancer survivors between 2014-2020. Prevalence estimates and Mantel Haenszel prevalence ratios were used to evaluate associations of race, ethnicity, and experienced racism with adverse psychosocial outcomes including days of poor mental and physical health, activity limitations, depression, and inadequate sleep. Experienced racism was framed as negative physical and emotional symptoms in reaction to perceived racism. Where sample size allowed, results were adjusted for age, sex, and education.
Results: Non-Hispanic Black, Hispanic, American Indian, Alaska Native, Native Hawaiian, and Pacific Islander survivors were more likely to experience at least one adverse outcome assessed in this study in comparison to non-Hispanic White (NHW) survivors. Specifically, non-Hispanic Black (NHB) survivors were 1.46 (95% CI:1.39, 1.54) times more likely, and Hispanic survivors were 1.16 (95% CI:1.07,1.25) times more likely than NHW survivors to report inadequate sleep after adjustment for age, sex, and education (Table 1). NHB survivors were 1.11 times more likely to report poor mental health (95% CI:1.01,1.21), and 0.91 times less likely to be diagnosed with depression than NHW respondents(95% CI:0.84,0.97). Distress secondary to racism was rarely reported however those who experienced racism-related distress reported a high burden of adverse health outcomes. Of those who experienced physical or emotional distress secondary to racism, 32-59% reported one of the studied adverse health outcomes (Table 2). Survivors reporting experienced racism were at greater risk to report each adverse health outcome included in this study in comparison to survivors who had not experienced racism with statistical significance in an unadjusted analysis.
Discussion: This study builds on the evidence that disparities in physical and mental health outcomes exist for cancer survivors of all ages from historically marginalized racial and ethnic groups. Specifically, our findings suggest NHB and Hispanic survivors may benefit from interventions targeted to assess and improve sleep and mental health. Additionally, experiencing physical or emotional symptoms of racism is associated with adverse physical and mental health outcomes in this cancer survivor cohort. Providers who care for cancer survivors may consider screening for experienced racism, a risk factor for adverse health outcomes.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal